Table of Contents
What is an Elimination Diet
An elimination diet is an organized way to remove potentially problematic foods from someone’s diet. If you’re suffering from digestive problems, an elimination diet should be one of the first things you try.
Because food sensitivities and food allergies are more common now than ever, elimination diets can be effective for many people (1).
Elimination diets are non-invasive, low cost, and pose a very low risk of harm.
There are several different elimination diets to choose from. This blog post aims to provide information and resources on the best elimination diets. We also discuss who is and is not a good fit for each elimination diet.
When is an Elimination Diet Helpful?
Adverse food reactions can cause symptoms just about anywhere in the body! If you have symptoms that don’t seem to resolve with conventional approaches and can’t otherwise be explained, it might be worth trying an elimination diet to see if you can get some relief.
Common symptoms of adverse food reactions include:
- Fatigue
- Insomnia
- Anxiety
- Mood swings
- Food cravings
- Brain fog
- Headaches
- Migraines
- Tinnitus (ringing in the ears)
- Sensitivity to sound
- Rashes or hives
- Eczema or psoriasis
- Flushing
- Itchy skin
- Sinus issues
- Canker sores
- Lung congestion
- Red, swollen, watery, or itchy eyes
- Sensitivity to light
- Urinary tract issues
- Joint pain or stiffness
- Muscle pain, spasms, or cramps
- Irregular heartbeat
- High blood pressure
- Heartburn or reflux
- Stomach or intestinal pains or cramps
- Constipation
- Diarrhea
- Bloating
- Gas or burping
- Nausea
- Vomiting
- Painful elimination
- Fluctuating weight
- Water retention
How to Do an Elimination Diet
The Elimination Phase
During the elimination phase of an elimination diet, foods suspected to be problematic are removed for some time and then reintroduced when symptoms have improved.
And by removed, we mean REMOVED! Even very small amounts of problematic food can cause symptoms. So we’re sorry, but that low dairy diet you tried wasn’t dairy-free. 😉
For someone with food sensitivities or food intolerances (which you’re about to learn are two different things), removing problematic foods can help manage symptoms.
Why you may feel worse when starting an elimination diet
- When problematic foods are removed, the body finally gets a break from the damage caused by inflammation. It can now get to work to heal and repair. Healing and recovering require energy, which can leave you feeling quite tired.
- Certain foods, like gluten, dairy, and soy, can have an opioid-like effect causing us to feel good when we consume them. If they’re also problematic, the opioid effect can mask their negative impact on our bodies. When these foods are removed, and that opioid effect is gone, we’re left to heal and recover without the pain-reducing effect (2).
- Some foods (like those with a high glycemic index) increase the production of serotonin and endorphins; when we stop consuming them, the production of these “feel-good” hormones decreases (3).
How long does it take to get results on an elimination diet?
If you don’t get any improvement within two weeks, it’s safe to say your diet isn’t working. Elimination diets aren’t meant to be permanent. They should be used as a tool to get symptoms under control and establish a healthy baseline.
The Reintroduction Phase
With every elimination diet, the elimination phase should be followed by a reintroduction phase.
Once the problematic foods have been removed (assuming you removed all of the right things and did so correctly), you should feel significantly better.
The goal should be to systematically liberalize your diet as much as possible, only avoiding what is necessary.
You’ll likely be able to tolerate some of what was removed and easily identify the truly problematic foods when you add them back in.
Adding foods back is an experiment to help you figure out what made you feel bad (so you will be looking to provoke symptoms upon reintroducing foods).
During the reintroduction phase, keeping a food journal and tracking your symptoms are important. This helps to identify patterns so you can figure out which foods are problematic for you!
If you cannot reintroduce any of the eliminated foods, other interventions and further testing might be necessary to find and address the root cause of your symptoms.
Food and Symptom Tracking Resources:
- My Symptoms App
- Cara Care App
- The food and symptom journal we provide to our clients – this is an old-fashioned handwritten journal with great instructions for tracking symptoms!
Elimination Diet Side Effects
Elimination diets should be used short-term to determine if food is causing adverse reactions. Following an elimination diet for long periods can have unwanted consequences.
- Whenever someone is following a restricted diet, nutrient deficiencies can occur.
- It’s important to test for nutrient deficiencies if you’ve been on an elimination diet for a long time (several months or more) because vitamin and mineral deficiencies can impair the body’s natural ability to heal.
- Another potential side effect of being on an elimination diet is unwanted stress. Sometimes removing food from someone’s diet can make them feel worse due to the emotional aspect of following dietary restrictions.
- Additionally, following a restricted diet for too long could lead to unwanted weight loss.
Help! My elimination diet isn’t working!
An elimination diet can be an effective way to address various health issues. Sometimes it’s enough, and sometimes more digging needs to be done.
If your elimination diet isn’t working, here are a few things to troubleshoot:
- Did you remove the wrong foods? Were you guessing at the foods, or did you have testing done? The right test can save a lot of time and guesswork!
- Are you accidentally eating something you’re sensitive or intolerant to – some foods are everywhere (think: gluten, dairy, FODMAPs, corn)! Check out our blog post on corn as an example – Corn Allergies and Sensitivities.
- Have you developed additional sensitivities?
- Do you have underlying issues causing the adverse reactions that have not been addressed? These can include SIBO, candida, low stomach acid, and dysbiosis to name a few.
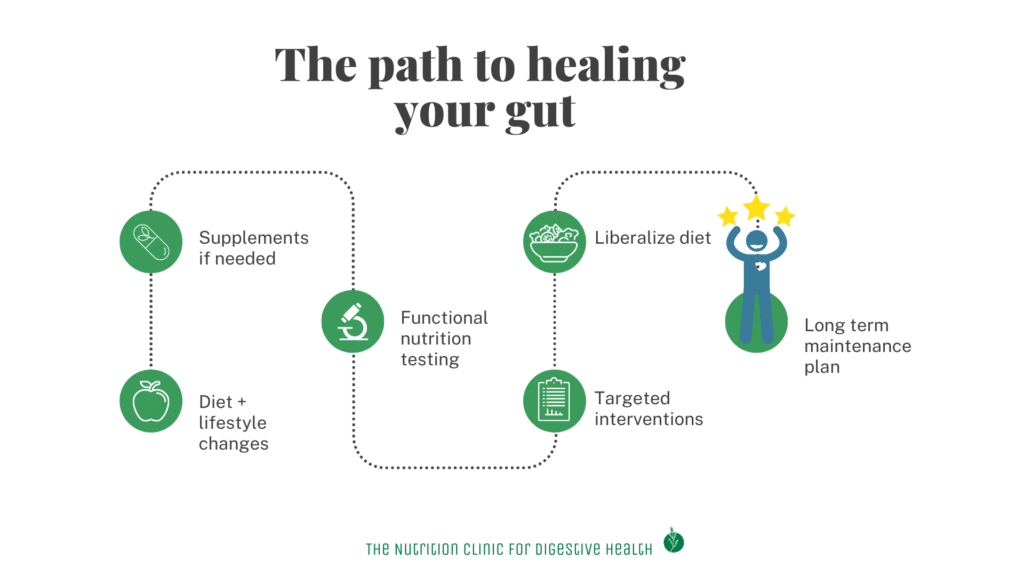
If you’ve considered all of the above troubleshooting tips and still don’t feel better, check out the graphic below.
Everyone’s path to feeling better looks different – some people do well with an elimination diet followed by a good probiotic. Others are more complicated and require a full workup of functional testing and heavier supplementation until they can get to the root cause of their digestive issues.
If an elimination diet isn’t enough to get you feeling better, digestive support can be added. This could include supplements such as enzymes, apple cider vinegar, gall bladder support, probiotics, and prebiotics.
If you can’t figure out the right amount of digestive support or supplements make you feel worse, it’s probably time to add in some functional nutrition testing. You can follow a targeted intervention based on your test results.
The Differences Between Food Allergies, Food Intolerances, and Food Sensitivities
Although these terms are used interchangeably, there are big differences between food allergies, food intolerances, and food sensitivities.
Here’s a reference chart highlighting the main differences; additional information can be found below.
| Immune System Involvement | Common foods | Onset of symptoms | Common Symptoms | Treatment | Testing | |
| Food Allergy | IgE antibodies, mast cells, pro-inflammatory mediators | Milk, Egg, Peanut, Soy, Wheat, Tree nut, Shellfish, Fish, Sesame | Within minutes to hours | hives, itching, diarrhea, trouble breathing, swelling | Avoid food completely – typically lifelong | Skin Prick Test |
| Food Sensitivity | IgG, IgA, IgM, pro-inflammatory mediators, White blood cells | Any food or chemical – can be dose dependant | Up to 72 hours after consumption | Can affect the entire body: Diarrhea, constipation, stomach pain, muscle and joint pain, seasonal allergy-like symptoms (runny nose and sneezing), fatigue, mental and emotional distress, brain fog, rashes, hives, headaches | Avoid for a period (typically 1-6 months) of time and then reintroduce – can change. | MRT |
| Food Intolerance | Not immune-mediated – related to not being able to break the food down properly | Lactose, histamine, FODMAP, sulfur | Varies from minutes to days | Bloating, diarrhea, constipation, stomach pain, greasy stool, excessive or odorous gas | Avoid for some time (typically 1-6 months) and then reintroduce – can change. | Testing for individual intolerance is available (ex: lactose tolerance test) |
Food Allergies
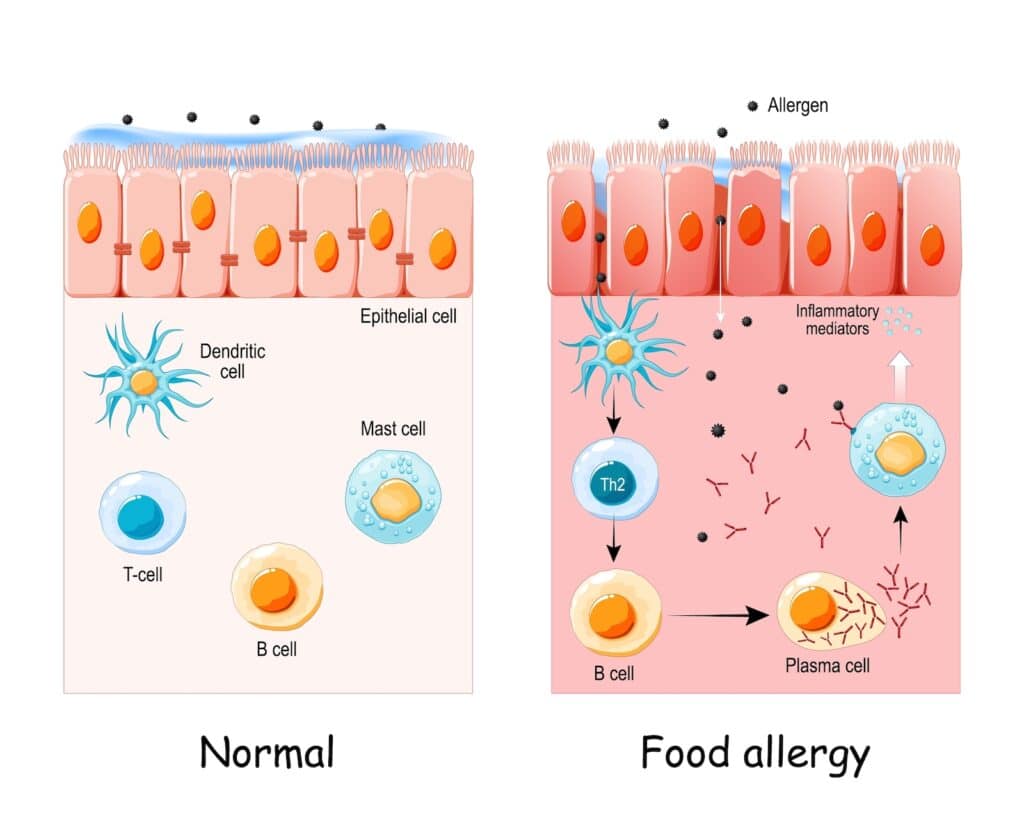
A food allergy is the body’s reaction to typically harmless foods that causes the immune system to produce IgE antibodies in response to proteins found in specific foods.
- Food allergies are typically considered to be life-long, and the food must stay out of the diet permanently.
- Sometimes people “grow out of” food allergies, but that’s more of an exception than the norm.
- When challenging allergenic foods, it’s recommended to be at the allergist with an epi-pen nearby.
- Unfortunately, hospitalizations due to food allergens have increased threefold since the 90s (4).
9 Most Common Food Allergies
Tree nut
Shellfish
Fish
Sesame
Egg
Soy
Milk
Wheat
Peanut
Food Sensitivities and Food Intolerances
Food Sensitivity
A food sensitivity occurs when the body begins an immune-mediated response to certain foods. Food sensitivities do not result in IgE antibodies (making them different from food allergies).
Food sensitivities involve the activation of the immune system, so a wide range of symptoms can develop.
Food Intolerance
A food intolerance occurs when your body has difficulty breaking foods down, resulting in digestive symptoms ONLY.
- Gas, bloating, diarrhea and constipation are symptoms of food intolerances.
- Intolerances are typically caused by a lack of enzymes (ex: lactose intolerance) or by the impact of chemicals (ex: histamine intolerance) and produce symptoms only in the GI tract.
Food sensitivities and intolerances can develop for several reasons (see below) but aren’t necessarily lifelong, and they don’t have the potential to become immediately life-threatening like a food allergy.
- Sensitivities and intolerances can change, lessen or go away completely once the body has healed.
- Also, food sensitivities and intolerances can be dose-dependent – meaning larger servings of food may provoke a symptom while smaller servings of that food do not produce any symptoms.
Food sensitivities and intolerances occur due to:
- Nutrient deficiencies
- The development of other diseases (such as Hashimoto’s or celiac disease)
- Bacteria, virus, fungus, or parasite infections
- Altered immune function
- Poor diet
Why Are Food Allergies on the Rise?
There are several theories for the increase in allergies and sensitivities:
Hygiene Hypothesis
- The “hygiene hypothesis” theorizes that due to less exposure to microbes and more sanitizing, the gut microbiome is not as robust anymore, resulting in more allergies.
- Children born via a C-section or given more antibiotics are MORE likely to have allergies due to not being exposed to bacteria when traveling through the birth canal (5).
- Children with older siblings and/or those that have pets early in life are LESS likely to have allergies since they are exposed to microorganisms at higher rates (6).
Dual Allergen Exposure Theory
The dual allergen exposure theory postulates that common allergen foods should be introduced early (between 5-11 months) during weaning to establish a tolerance (7).
- For many years, the recommendation was the opposite – parents were told to keep common allergen foods out of the diet, which could have led to an increase in allergy cases.
- Unfortunately, many parents still think this is the case and wait until age 2 or 3 to expose their kids to certain foods.
- Exposure to a wide range of foods as early as possible is now the recommendation by allergists.
Vitamin D Deficiencies
Vitamin D deficiencies, partially due to more time spent inside, have also been linked to an increased likelihood of food allergies (8). This is because vitamin D helps to regulate the immune system.
Interestingly, vitamin D levels shouldn’t get too high as this can also increase the development of food allergies (9).
We recommend monitoring your vitamin D levels with a goal of 50-80 ng/ml.
Increase in Chemical Exposure
In the common Standard American Diet (SAD as it is accurately called), we are exposed to many more chemicals now through the intake of processed foods than ever before. 🤮
The theory is that this increased chemical load alters the immune system by making the detoxification organs work overtime.
Food Sensitivity Testing
Since elimination diets can address food sensitivities, we’re reviewing food sensitivity testing here.
- We love food sensitivity testing because it’s super helpful! It takes the guesswork out of which foods are causing problems for our clients, helping them feel better faster. In the long run, testing saves you time, misery, and money.
- Because there are so many food sensitivity tests out there, it would take an entire blog article to explain the nuances of each.
- If you want to go further in-depth than we do here, check out Erica Julson’s article, which explains 11 different food sensitivity tests and their pros and cons.
- Below we’re giving a quick review of the most popular food sensitivity tests.
IgG Testing
Companies like EverlyWell and Pinnertest use IgG testing. IgG is the most widely available option because it’s very cheap and quick.
- While the tests accurately measure IgG presence, they are NOT clinically useful. Following these results can cause unnecessary food restrictions.
- IgG production is often a normal part of the immune system response to food consumption, so the presence of IgG does NOT necessarily = an inflammatory response, it can simply indicate that you recently consumed the food.
- It’s also been shown that when the immune system produces IgG in response to certain foods, it may actually protect you from an allergy to that food (10, 11).
- Many organizations, including the European Academy of Allergy and Clinical Immunology and the American Academy of Allergy, Asthma, and Immunology, do NOT recommend using this test as a diagnostic tool (12).
- We agree! In our practice, we view these tests more as glorified food journals than helpful information.
- Also, these tests do not assess chemical sensitivities, which can be a missing piece of the puzzle for those dealing with food sensitivities.
P88 Dietary Antigen Test
This test offered by Precision Point Diagnostics includes IgE, IgG4, and complement (C3d) testing along with IgG to measure allergies and sensitivities. Complement activation is thought to amplify the immune system’s response, resulting in more severe inflammation and symptoms (13).
While this test is a much better option than one solely measuring IgG, it’s not our favorite.
- Some IgG4 is beneficial against the development of allergies or sensitivities, whereas too much promotes inflammation (14).
- This test measures 88 foods but does not test for reactions to chemicals which again can be a missing piece of the puzzle for those dealing with food sensitivities.
MRT Food Sensitivity Test
MRT stands for Mediator Release Test. This is what we use in practice – when the test results are combined with the right dietary protocol, our clients get really good results.
Here’s why we love MRT for food sensitivities:
- It’s got the best technology behind the test. As the name implies, it measures mediator release (mediators cause inflammation and are the molecules responsible for producing food sensitivity symptoms).
- While no test is perfect, MRT is highly accurate. The sensitivity is 94%, and it’s 91% specific. Meaning there is a low chance of having a false positive or false negative in your blood test results.
- Also, a food sensitivity can occur without triggering antibodies (IgG, IgA, or IgM) and directly trigger white blood cells. This means IgG tests will miss the food sensitivities that occur via the white blood cell pathway.
- MRT measures 170 different foods and chemicals. The test panel includes chemicals that naturally occur in food and chemicals that are added to food.
- Here’s why testing for chemicals is so important: you can react to a chemical in a food and not the food itself on the testing panel. Reactivity to chemicals is often related to the dose. Meaning that the more of a chemical you consume, the more likely you are to react.
- Let’s take fructose, for example – the sugar naturally occurring in fruit. Being reactive to fructose doesn’t mean you can’t eat fruit. You may be able to eat two servings of fruit and be okay, but if you eat three servings, you might start to have a problem (like gas, bloating, or diarrhea).
- Here’s why testing for chemicals is so important: you can react to a chemical in a food and not the food itself on the testing panel. Reactivity to chemicals is often related to the dose. Meaning that the more of a chemical you consume, the more likely you are to react.
Scientific studies supporting the MRT test include:
- Validation of the testing process – white blood cells are monitored after exposure to an antigen to see how much they shrink in size. A decrease in cell size indicates that inflammatory mediators were released. The amount of cell shrinkage correlates with the severity of the food sensitivity.
- This study presented at the 2004 American College of Gastroenterology annual seminar showed a 53% improvement in IBS-Diarrhea symptoms after one month of participants following the LEAP protocol using their MRT results.
- Use of the LEAP Mediator Release Test to identify non-IgE mediated immunologic food reactions that trigger diarrhea-predominant IBS symptoms results in marked improvement of symptoms through the use of an elimination diet
The research process is long and tedious. We’re so excited to have more studies on MRT in progress. Currently, the following conditions are being studied using MRT as an intervention:
- Patients diagnosed with IBS
- Pediatric patients with Crohn’s disease
- Women with PCOS
- Patients with migraines
In our clinical experience (along with hundreds of other clinicians using MRT), using the results from this test dramatically reduces inflammation, decreasing symptoms for the majority of our clients.
According to the Academy of Nutrition and Dietetics, “when peer-reviewed scientific studies are lacking, we must rely on expert opinion and experience.”
Elimination Diet Plans
The timeline for an elimination diet varies based on the type of diet you choose, the severity of your symptoms, and your goals.
You might feel worse at the beginning of an elimination diet before you start to feel better. As we said before, if you’re not doing significantly better after 14 days, it’s time to reassess.
Now, let’s dive into the details on elimination diets we use and who they are appropriate for (and who they aren’t).
LEAP Food Sensitivity Testing Protocol
The LEAP Protocol is a personalized anti-inflammatory diet.
- The diet is based on your blood work using the Mediator Release Test.
- The test results show a color-coded bar graph (pictured on the right) corresponding to the degree of inflammation produced by food or chemical antigens.
- Most of the time, we recommend avoiding moderately reactive (yellow bar) foods for three months and highly reactive (red bar) foods for six months. They can then be tried again if desired to reassess tolerance.
Our dietitians work with clients to create a personalized elimination diet based on their test results.
- The collaboration ensures the diet will be doable and that easy meal and snack options are planned, enjoyable, and available. All of these pieces are needed so that the diet will be effective!
- The first phase of the diet lasts for two weeks. The goal of this phase is to calm down the immune system so that symptoms are alleviated.
- Our typical LEAP client has a 50% improvement in symptoms during this time! Success makes it easy to stay motivated and compliant.
- After the initial two-week period, you strategically add foods to your diet while monitoring your symptoms. We usually recommend adding in one new food every one to three days. As we explained previously, food sensitivity symptoms can take 72 hours to show up.
We recommend preparing all of your food at home for the first several weeks. This reduces the chances of cross-contamination and accidentally eating foods that aren’t on your plan.
Who needs a LEAP diet?
This is a good fit for you if you’re…
- Suffering from systemic symptoms (occurring outside the GI tract)
- Diagnosed with IBS or IBD
- Wondering if food is playing a role in your symptoms but can’t figure out which food is the problem
- Willing to give up any food for at least two weeks and alcohol for at least one month
- Not having success with other elimination diets
Is the LEAP diet good for everyone?
This isn’t a good fit for you if you’re…
- Recovering from an eating disorder
- Suffering from anxiety that’s triggered by restrictive diets
- Traveling often and can’t meal prep
- An extremely picky eater
- Currently on a strict diet and have been severely limiting foods for six months or more.
- Not willing to give up foods you love
LEAP MRT Resources
Low FODMAP Diet
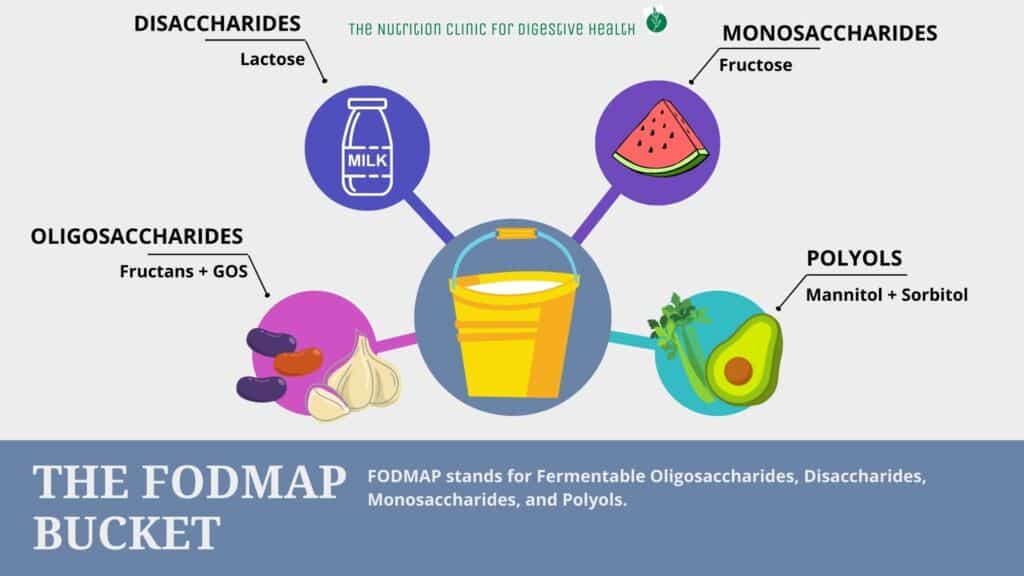
FODMAP is an acronym for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols, which are different groups of carbohydrates consumed in most diets.
Each FODMAP group is further broken down, and specific foods fall into the sub-categories. Oy!
Here are a few examples to make this more relatable (this is not a full listing for each group).
| Oligosaccharides (Fructans + galacto-oligosaccharides (GOS)) Wheat, barley, rye, onion, garlic, beans | Monosaccharides (Fructose) Pears, honey, apples |
| Disaccharides (Lactose) Milk, ice cream, cottage cheese | Polyols (Mannitol + sorbitol) Sugar-free gum, avocado, corn, mushrooms, cauliflower |
- High FODMAP foods aren’t well absorbed in the small intestine, which is why they cause digestive problems.
- Because FODMAP-containing foods aren’t well absorbed, they can hold excess fluid in the gut, causing bloating and stomach pain (16).
- Also, because these carbohydrates are fermentable, they naturally produce excess carbon, hydrogen, and methane gasses as a byproduct, ultimately resulting in digestive symptoms. This is also why foods like cabbage, beans, and broccoli cause bloating for just about everyone.
- Diarrhea, bloating, gas and constipation are symptoms of FODMAP intolerance.
- A high FODMAP diet can increase gut permeability by increasing bacteria, and promoting inflammation.
- Removing FODMAPs only addresses food intolerances, not food sensitivities. If you have symptoms occurring outside of the GI tract, MRT may be a better fit for you.
Removing high FODMAP foods from the diet has been shown to greatly relieve GI symptoms for individuals with:
- IBS (18, 19, 20)
- IBD (21, 22, 23)
- SIBO (24, 25)
- *Even though a low FODMAP diet has not been researched directly on patients with SIBO (probably due to lack of funding), as practitioners, we can connect the dots from the data that we do have. We do know that a low FODMAP diet can lower certain strains of bacteria, and we know that it improves IBS symptoms. We also know that one of the root causes of IBS is SIBO. Therefore, we feel comfortable recommending a low FODMAP diet for clients with SIBO.
- Exercised induced GI symptoms (26, 27)
- Fecal Incontinence (28)
How to Do Low FODMAP diet
Following a low FODMAP diet means you are keeping your total FODMAP load to a minimum by limiting high FODMAP foods.
To explain this process, picture a bucket.
Each time you eat, you add FODMAPs to your bucket. When your bucket overflows, digestive symptoms occur.
It’s very much a dose/response relationship.
To stay organized and clear on how FODMAPs affect you, this diet is divided into phases.
FODMAP Elimination Phase
During this phase, you eliminate high FODMAP foods.
- The goal of this phase is to reduce the amount of FODMAPs you put into your bucket to hopefully reduce your symptoms.
- Depending on your symptom resolution, the elimination phase can last anywhere from 4 weeks to several months.
- We do NOT recommend staying in the elimination phase indefinitely due to the inherent lack of prebiotic foods, which can negatively alter the gut microbiome (29).
FODMAP Reintroductions – the challenge phase
When you add FODMAPs back to your diet in the challenge phase, you’re trying to determine how many FODMAPs you can fit into your bucket before it overflows.
The ultimate goal is to get you feeling your best with the least amount of dietary restrictions.
- During the challenge phase, you reintroduce the different groups of FODMAPs one at a time.
- For highly sensitive people, this looks like adding in one FODMAP group every week with a 3-day wash-out period in between reintroductions to assess for symptoms.
- For less sensitive people, you might be able to reintroduce the groups quicker.
Having an intolerance to one or two groups of FODMAPs isn’t reason for concern (especially if one of them is lactose).
If you can’t tolerate any high FODMAP foods after the elimination phase, you’ll need to do more digging to address the root cause of your FODMAP intolerance.
Because this can be a difficult diet to follow correctly (and reintroduce correctly), we recommend working with one of our registered dietitians to get the best results.
Underlying causes of FODMAP intolerance include:
- SIBO
- A parasite Infection
- Lack of digestive enzymes
- Low stomach acid
- Celiac disease
Who needs a Low FODMAP diet?
This is a good fit if you…
- Only have digestive symptoms.
- Have been diagnosed with IBS, IBD, SIBO, exercise-induced GI symptoms, or fecal incontinence
- Struggle with constipation, diarrhea, stomach pain, gas, and/or bloating
Is a Low FODMAP diet good for everyone?
This isn’t a good fit if you…
- Have digestive symptoms and systemic symptoms (symptoms occurring outside the GI tract)
- Don’t have time for food prep
- Travel frequently
- Enjoy dining out often
Low FODMAP Resources
Of all the diets we counsel clients on, this is the one people think they are following correctly but usually aren’t.
Getting portion sizes right on this diet is critical to success, as is following trusted resources. Several FODMAP resources are out there, and many conflict with each other.
Before you give up following a low FODMAP diet, consider working with a professional (such as one of our dietitians) with FODMAP diet experience.
- FODY Foods – low FODMAP sauces, condiments, spices, oils, and snacks
- Modify Health – low FODMAP freezer meal delivery service
- Use code DIGESTIONTHERAPY for $60 off your first three weeks and free shipping!
- Low FODMAP Snacks
- Monash University Low FODMAP Recipes
- Kate Scarlata Low FODMAP Recipes
- Which Foods are High or Low in FODMAPS?
AIP Elimination Diet
The autoimmune protocol diet (or AIP), developed by Dr. Sarah Ballantyne, is a more restrictive version of the commonly used Paleo diet. Going beyond the Paleo diet of eliminating grains, dairy, and legumes, the AIP diet also removes foods suspected to contribute to autoimmune issues.
- It’s important to understand that this can be very helpful for some, but it’s a generalized plan. While we do support the AIP diet and use it in practice for some people, food intolerances and sensitivities do vary from person to person, which is why we prefer MRT.
- The theory is that the foods removed (see next section) contribute to inflammation and dysbiosis. Inflammation and dysbiosis contribute to autoimmune conditions and exacerbate symptoms in an already taxed body.
- Although research is limited, the available research shows very good results using the AIP diet in people with Hashimoto’s thyroiditis, Crohn’s disease, and ulcerative colitis. (29, 30, 31) .
- We ❤ that this protocol emphasizes what you can eat and focuses on nutrient-dense foods like bone broth, non-dairy fermented foods, and organ meats.
AIP Elimination Phase
- The timeline of the elimination phase is based on symptom severity. It’s recommended not to move into the reintroduction phase until your symptoms are mostly under control.
- The elimination phase is recommended for at least four weeks and no longer than three months.
- Foods removed during the elimination phase of the AIP diet include:
| Grains | Artificial sweeteners | Nuts and seeds | Coffee |
| Eggs | Nightshade vegetables* | Dairy | Alcohol |
| Legumes | Overly processed oils | Food additives | NSAIDS |
* Nightshade vegetables include tomatoes and tomato-based foods and products, tomatillos, potatoes, eggplant, peppers (bell peppers, jalapeno, chili peppers, and hot peppers), red spices (curry powder, chili powder, cayenne powder, red pepper, paprika), pimentos, tobacco, goji berries, ground cherries, and ashwagandha).
If you’ve been on the AIP diet for three months and still have symptoms, it is time to meet with one of our registered dietitians to help identify missing links!
Who needs the AIP diet?
This is a good fit if you…
- Have an autoimmune condition or suspect an autoimmune condition due to chronic symptoms like muscle pain, excessive fatigue, and joint pain
- Are willing to prepare your food
- Have tried other elimination diets before with some success but not full symptom improvement
- Don’t have the budget for MRT food sensitivity testing
- Felt worse on the Whole 30 Elimination Diet (usually due to increased intake of eggs, nuts, and seeds)
Is the AIP diet good for everyone?
This isn’t a good fit if you…
- Have an eating disorder, are underweight, or are triggered by restrictive diets.
- Don’t suspect an autoimmune disorder.
- Follow a vegan diet – this is due to an increased risk of nutrient deficiencies since this protocol limits most plant-based protein sources.
AIP Elimination Diet Resources
There are so many amazing resources out there for the AIP diet; here are a few of our favorites:
- Autoimmune Wellness
- The Paleo Mom
- Phoenix Helix Recipes
- Real Plans – an AIP-compliant meal planning service
Whole 30
The Whole 30, created by Melissa Urban, is a very common elimination diet that cuts out foods associated with food sensitivities (i.e., gluten and dairy) and food intolerances (i.e., beans and legumes and soy).
- It’s important to understand that this can be very helpful for some, but it’s a generalized plan. While we do support Whole 30 and use it in practice for some people, intolerances and sensitivities do vary from person to person, which is why we prefer MRT.
- Whole 30 is less restrictive than the AIP protocol – keeping eggs, coffee, nuts, seeds, and nightshade vegetables in the diet.
- Another benefit of Whole 30 is that it’s been around for over a decade, so there are lots of resources that make it easier to do. You can even find products in the grocery store with a Whole 30 seal of approval that work on this elimination diet.
- Although there isn’t any peer-reviewed research specifically on the Whole 30, there’s research to explain why each food group is eliminated. There are also thousands of real-life testimonials.
Phases of Whole 30
- There’s a 30-day elimination period followed by ten days of reintroductions, which can be done at a slower pace if desired.
- During the elimination phase, you’re instructed to avoid weighing yourself or taking measurements of any kind.
- The foods removed during the elimination phase are listed below
| Foods Removed | Reason for removal |
| Grains (32, 33) | Can increase gut permeability and be hard to digest |
| Legumes (34) | These are high FODMAP which makes them difficult to digest |
| Dairy (35) | 60-70% of the world has lactose intolerance |
| Added Sugar (36) | Increases cravings, alters blood sugar, competes with the consumption of nutrient-dense food, associated with inflammatory conditions |
| Alcohol (37) | Large amounts can damage the GI tract |
| Added chemicals (carrageenan or sulfites) | Found in processed foods, which promote inflammation and lack nutrients |
Who needs the Whole 30 diet?
This is a good fit if you…
- Dine out or travel often and want to try an elimination diet
- Follow a vegan diet and have digestive symptoms (there’s a specific plant-based Whole 30 plan)
Is the Whole 30 diet good for everyone?
This isn’t a good fit if you…
- Have an eating disorder, are underweight, or are triggered by restrictive diets.
Whole 30 Recipes and Resources
- Meal Planning and Recipes
- Meal Delivery and Restaurants
- Dressings
- Books and Cookbooks
- Plant-Based Whole 30 Rules
Healing Gut Diet
We designed the Healing Gut Diet with our clients in mind 😃.
This diet removes foods that make it difficult for the gut to heal and adds in foods that are easy to digest and anti-inflammatory.
Anti-inflammatory foods on this meal plan include:
- Foods rich in omega-3 fatty acids like fatty fish, chia seeds, and walnuts
- Antioxidant-rich foods like leafy greens and berries
- Protein-rich foods like eggs, chicken, and shrimp
- Healthy fats like canned coconut milk and avocado
- Collagen and glutamine-rich foods like bone broth and beef roast
For a more detailed description of why we recommend removing the foods in the chart below, start with our blog post on the Healing Gut Diet.
| Remove | Replacements |
| Gluten | Quinoa, oats, rice, corn |
| Dairy | Nut milk alternatives |
| Added Sugar | Cacao nibs, freeze dried fruit |
| Raw Veggies | Cooked vegetables, soups, slow cooker meals, smoothies |
| Alcohol | Collagen Peptides, Bone broth, Gelatin |
Because it can take anywhere from three months to a year for someone’s gut to heal and because you’re not at risk for nutrient deficiencies, you can stay on this diet longer than others described in this post.
We recommend starting with one month, and if you do not feel significantly better, then it is time to get support from one of our registered dietitians.
Who needs the Healing Gut Diet?
This is a good fit if you…
- Have had physical damage to your GI tract
- Recently had food poisoning, a flare in GI symptoms, or need a gut reset
- Struggle with unwanted GI symptoms
- Need an affordable diet plan to heal your gut
- Are busy without much time for food prep
- Travel often
- Have never tried an elimination diet before
Is the Healing Gut Diet good for everyone?
This isn’t a good fit if you…
- Struggle to have a healthy relationship with food
- Aren’t willing to make dietary changes
Resources
Gluten-free and Dairy-free
Lastly, we wanted to touch on the most basic elimination diet, going gluten-free and dairy-free.
- While this can seem daunting, our clients find it easy to make these changes with the right resources.
- If you’ve never tried eliminating gluten and dairy from your diet, we recommend giving it a shot for at least four weeks. Then, you can reintroduce each one at a time and see how your body feels.
Common sources of gluten
Gluten-containing grains
Be sure to read food labels and avoid these ingredients when eliminating gluten:
- Barley
- Barley malt/extract
- Bran
- Bulgar
- Couscous
- Durum
- Einkorn
- Emmer
- Farina
- Farro
- Graham flour
- Kamut
- Matzo flour/meal
- Orzo
- Panko
- Rye
- Seitan
- Semolina
- Spelt
- Triticale
- Udon
- Wheat
- Wheat bran
- Wheat germ
Hidden sources of gluten
Some of the above may seem like obvious sources of gluten. But, gluten can also be sneaky – lots of times, it’s hiding in foods and even non-food products that you may not suspect.
Food products that can contain gluten:
These may or may not contain gluten, label reading is essential to ensure you’re gluten-free. Companies can change ingredients in their products, so be sure to check labels often.
| Ale | Stuffing | Breading |
| Beer and lagers | Bread crumbs | Self-basting poultry |
| Soup bases (like bouillon cubes) | Pasta | Brown rice syrup |
| Drink mixes | Broth | Cured pork products |
| Lunch meat | Soy sauce | Communion wafers |
| Marinades | Croutons | Imitation meat |
| Seafood coating mix | Gravy | Sauces |
| Thickeners | Cakes, cookies, doughnuts | Ice cream cones |
Non-food products that can contain gluten:
These may or may not contain gluten, it’s advised to check the ingredient labels to ensure you’re gluten-free.
| Supplements | Playdough |
| Medications (prescription & OTC) | Lipstick, lip gloss, chapstick, lip balm |
| Lotion | Stamps and envelope glue |
| Mouthwash & Toothpaste |
Common sources of dairy
Dairy doesn’t require quite the diligence gluten does to remove from your diet. However, the list below is still worth reviewing. Be sure to avoid these when eliminating dairy:
| Milk | Butter | Ghee |
| Cream | Yogurt | Kefir |
| Half & half | Whey | Casein |
| Sweets * (chocolate, baked goods, packaged foods) | Cottage cheese | Protein bars* |
| Granola bars* | Whey protein powder |
*may contain dairy
Who needs a Gluten-free and Dairy-free Diet?
This is a good fit if you…
- Currently eat a lot of processed food, fast food, sugar, and/or soda
- Are on a strict food budget
- Are too busy to prepare food
- Have anxiety around food or a history of an eating disorder
- Travel often
- Struggle with unwanted GI symptoms
Is a Gluten-free and Dairy-free diet good for everyone?
- This diet is appropriate for almost everyone with GI symptoms 🙂
- One thing to note: We recommend testing for celiac disease before completely pulling gluten from your diet.
Conclusion
We always recommend starting with diet and lifestyle changes when trying to heal your gut.
Sometimes, an elimination diet is all you need to feel better. But, sometimes, an elimination diet isn’t enough. That’s when it becomes time to look for underlying imbalances that need to be addressed.
Underlying imbalances that cause adverse food reactions can include:
- Gut dysbiosis
- Bacterial, viral, parasite, or fungal Infections
- Environmental toxins
- Certain medications
- Inadequate liver function
- Poor thyroid function
- Gallbladder removal
- Long-term PPI use
When the body is balanced, and the gut is healthy and functioning the way that it should, food shouldn’t cause problems.






Leave a Reply