Table of Contents
Why is self-care important for autoimmune diseases?
Self-care is super important for everyone, but it’s particularly important for people with autoimmune diseases.
Self-care practices can help individuals with autoimmune diseases manage their symptoms, improve their quality of life, and even reduce the risk of flares by lowering stress and calming down chronic inflammation.
Research shows that proper self-care can lead to better management of autoimmune diseases. For example, research has proven that self-care can help alleviate autoimmune symptoms, make you feel better, and give you a better outlook on your body and disease.
Let’s shift our perspective on self-care from a list of things we need to buy, like the newest bath bomb or face cream (although these things can be wonderful), to a celebration of kindness towards our bodies. While managing autoimmune conditions can be demanding, remember that every act of self-compassion counts. You’re doing great!
Self-care habits
Defining what self-care is for you will be different than someone else. Regularly going to yoga classes or getting massages might work for you.
But you might find yourself in a season of life where those commonly talked about self-care to-dos aren’t as helpful, and you need tools that are readily accessible and will help you care for your body every day.
Our intent with today’s article isn’t to give you another checklist of more things to do but rather to give you ideas that will help you care for yourself in little ways every day!
What is celiac disease?
Celiac disease is an autoimmune disease. Autoimmune diseases occur when the body’s immune system mistakenly attacks healthy tissues and organs, leading to chronic inflammation and damage to various parts of the body.
People with celiac disease have an autoimmune response to gluten. When someone with celiac disease eats food containing gluten, the immune system’s response leads to damage in the small intestine.
Gluten is a protein found in wheat, rye, and barley.
What happens when someone with celiac disease eats gluten?
The damage that occurs to the small intestine when someone with celiac disease eats gluten can lead to various symptoms. These include:
- Diarrhea or constipation
- Abdominal pain
- Nausea and vomiting
- Gas
- Extreme fatigue
- Muscle and joint pain
- Mental health issues
- Problems with the menstrual cycle, including infertility
- Nervous system issues such as tingling, headaches, and numbness
- Skin rashes
Hidden symptoms of celiac disease
While some of the above symptoms are relatively common for someone to experience if they have celiac disease, some symptoms are harder to identify and often are due to celiac disease as well. Some of these hidden symptoms include:
- Anemia, usually from iron deficiency
- Loss of bone density (osteoporosis) or softening of bone (osteomalacia)
- Blistery skin (dermatitis herpetiformis)
- Mouth ulcers
- Reduced functioning of the spleen (hyposplenism)
Over time, this damage creates a cascade of health issues as the microvilli are damaged. Microvilli are fingerlike projections inside the small intestine that absorb nutrients. When they’re damaged, nutrient deficiencies can occur.
The most common micronutrient deficiencies for people with celiac disease include iron, B vitamins, vitamin D, copper, and zinc.
Celiac disease has no cure, but symptoms can be managed by following a strict gluten-free diet.
Celiac disease versus non-Celiac gluten sensitivity (NCGS)
Non-Celiac Gluten Sensitivity (NCGS) is a condition that is often confused with Celiac because the symptoms can be very similar. As stated earlier, when someone with Celiac disease ingests gluten, their body’s immune system doesn’t recognize it and antibodies begin to attack their intestinal lining, which causes damage.
However, with NCGS, this immune reaction does not lead to small intestine damage. While the symptoms that present are extremely similar, Celiac disease is much more severe and requires constant surveillance to prevent gluten exposure from places that are not commonly looked at (like not using the same knife as your friend buttering their toast).
From a dietary perspective, the main difference is that someone with celiac disease should never have any amount of gluten. Someone with NCGS can likely tolerate a small amount of gluten and be okay afterward or doesn’t need to be as concerned about cross-contamination (this is not to say that we would ever recommend it or, in good conscience, give someone with NCGS an OK to consume gluten). Symptoms in someone with NCGS likely wouldn’t be as severe as they would in a person with celiac disease.
However, since gluten is so hard to avoid, we do recommend that those with NCGS try to avoid it completely. This is because no matter how hard you try to avoid eating gluten, you are likely going to be exposed to it. This is either from dining out or just honest mistakes made in day-to-day life!
Avoiding it consistently can help make these intermittent exposures cause fewer symptoms in someone with NCGS. The more gluten someone consumes with celiac or NCGS, the more severe the response to the gluten would be. Symptoms and severity will be different for everyone, but generally, it’s best practice to avoid gluten completely for both Celiac and NCGS.
Celiac Disease Self-Care Guide
Now that you have a thorough understanding of Celiac Disease, we have created the most extensive guide on the internet on how to practice self-care with celiac disease! Keep reading for the step-by-step guide.
1. Understand which foods contain gluten
This may sound obvious, but it takes some time to learn. Gluten is just about everywhere! Many clients come to us for help navigating gluten-free diets after being diagnosed with celiac or non-celiac gluten sensitivity.
If you or a loved one needs support following a gluten-free diet, click here to schedule a FREE 15-minute call with one of our dietitians today to learn more about working with us.
Foods to avoid on a gluten-free diet
The grains below contain gluten and should be avoided by people diagnosed with celiac disease and NCGS.
- Barley (all forms, including barley malt and extract)
- Bran
- Bulgur
- Couscous
- Durum
- Einkorn
- Emmer
- Farina
- Faro
- Graham flour
- Kamut
- Matzo flour and meal
- Orzo
- Panko
- Rye
- Semolina
- Seitan
- Spelt
- Triticale
- Udon
- Wheat
Hidden sources of gluten
Gluten can “sneak” into many places – the foods below commonly contain gluten and should be avoided for someone with celiac disease.
- Beverages – Malted milk ( for example, Ovaltine), ale, beer, and even instant coffee can have wheat flour added!
- Sauces and condiments – Beware of soy sauce, bouillon cubes, English mustard, salad dressings, BBQ sauce, ketchup, and tartar can contain gluten so always check labels carefully!
- Breads and baked goods – Anything made with wheat, rye, kamut, spelt, or barley will contain gluten. Pancakes, muffins, biscuits, waffles, crackers, pretzels, bread crumbs, breaded or fried foods will also contain gluten unless declared gluten-free.
- Cereals – Any made with wheat, rye, kamut, spelt, barley, wheat germ, or triticale will not be gluten-free.
- Meat, Fish, Eggs, Cheese – Avoid breaded meat, poultry, fish, patties, croquettes, and loaves containing bread crumbs. Also be sure to check canned meats, cold cuts, and hot dogs. Additionally, creamed sauces, gravies, and spreads can contain gluten. Even scrambled eggs can be thickened with flour!
- Potatoes and Pasta – Be sure to find gluten-free alternatives for spaghetti noodles, macaroni, dumplings
- Vegetables – Any prepared with bread crumbs or cream sauces are likely to contain gluten
- Desserts – Commercial ice creams, ice cream cones, prepared pudding mixes, homemade puddings thickened with flour, cake, cookies, doughnuts, pies, and pastries normally contain gluten.
2. Be aware of cross-contamination
Someone with celiac disease must be completely (yes, 100%) gluten-free. Even the tiniest amount of gluten can trigger a negative response (we’re talking even breadcrumbs).
Along with avoiding gluten, people with celiac disease must be aware of cross-contamination.
Cross-contamination is when a non-gluten-containing food comes into contact with gluten during preparation. This can happen in many settings both at restaurants and at home, during cooking, or when food is stored.
An easy example is someone toasting gluten-free bread in a toaster just used for regular bread. The leftover breadcrumbs coming into contact with the gluten-free bread are enough to cause problems in someone with celiac disease.
This is also why restaurants may hesitate to declare gluten-free items unless they have a separate space for preparation.
Tips to avoid cross-contamination
Anyone with celiac disease must have separate utensils, cooking surfaces, and appliances if they share a home with people who consume gluten to avoid cross-contamination.
When dining out, asking questions about ingredients and food preparation methods is essential.
For example, if you order something fried and it’s cooked in the same fryer as gluten-containing foods, the fryer is contaminated, and your gluten-free fried food is no longer safe.
3. What do I do if I accidentally eat gluten?
Accidentally ate gluten and want to know how to feel better? No matter how hard you try to avoid gluten, it’s everywhere, and you’ll likely need a gluten-remedy at some point, especially if you travel or dine out frequently. Here are a few tips that could help:
- Hydrate! Drinking a lot of water after accidentally eating gluten can help to flush your digestive system and help eliminate whatever you consumed. This can also help replenish fluids to prevent dehydration if you experience diarrhea.
- Set aside time to rest. Unfortunately, if you have celiac disease, you are likely going to feel the effects of consuming gluten pretty quickly after eating it. While you may be frustrated, give yourself grace and set aside time to let your body rest. Lay in your bed, and put on your favorite show. It will pass, and you will soon feel well again.
- Consider supplementation. Supplements like digestive enzymes can help break down the food in your system (including the gluten you consumed) and lessen the severity of your symptoms.
- Give your digestive system a break. At some point, you’re going to need to eat while you’re recovering from getting glutenated. Of course, we know to continue avoiding gluten, but when trying to eat, focus on eating easy-to-digest foods like broth, rice, bananas, and gluten-free crackers. Avoid eating a large meal until you feel better.
- Book a consultation with us! Accidentally eating gluten is scary, and we are here to help. Feel free to book a one-time consultation with one of our gut health experts if you want to figure out how to ease your symptoms and prevent this from happening in the future.
4. Advocate for yourself and your dietary needs
You will be your best advocate. Instead of thinking about your allergy as a hassle for other people, remind yourself that you deserve to feel good just like everyone else does, and keeping gluten out of your diet is how you do that.
This could look like bringing your own food to work or dinner parties.
Or, if someone offers to prepare food for you, be sure to inform him or her about your dietary needs and cross-contamination to prevent accidental gluten exposure.
Be sure to utilize the many gluten-free resources out there; here are some of our favorites:
- The Find Me Gluten Free app helps find restaurants close to you with gluten-free options.
- Gluten-Free Goddess Blog – gluten-free recipes
- Cook Once Eat All Week – a cookbook with 26 weeks of gluten-free meal prep
5. Seek social support
Ask for specific help when and where you need it. Many meal delivery services offer gluten-free foods to help you in this new lifestyle.
If you’re not yet comfortable speaking to the chef or manager if you are at a restaurant, ask your partner or dinner companion to do it for you.
Facebook groups can help you feel like you are not alone on your health journey.
6. Set boundaries
This can be especially hard if you tend to be a people pleaser. When you have celiac disease (or any other autoimmune disease), your body needs more rest, and preserving your energy by saying no can help.
The truth is that we don’t need to be everything for everybody. It’s easy to get caught up in saying yes to everything. Saying no is a powerful tool and a way you can care for your body.
Avoiding overcommitting can also help you carve out time to give a yes to something you really care about.
When you’re first diagnosed with celiac disease, saying no to eating at certain restaurants can be critical to keeping gluten out especially if you are tempted to partake. Let’s say a friend invites you to her birthday party at a restaurant that doesn’t have any strictly gluten-free offerings. You could tell that friend that you can’t come to her event, but you would love to celebrate their birthday in another way together.
7. Explore a hobby or passion
Find something to do that brings you joy (away from the things you HAVE to do daily).
This could be starting a small herb garden or trying your hand at a new skill like learning to play piano.
If you’re reading that and thinking, where will I find the time, consider the concept of activity stacking. Activity or habit stacking from Atomic Habits by James Clear is the idea of doing this new thing at the same time you are doing something else you already do (i.e. instead of meeting friends for dinner, start a book club together)
8. Cultivate self-compassion
Self-compassion is the habitual act of relating to yourself in a gentle and kind way when faced with feeling inadequate.
Practicing self-compassion can improve our ability to cope with life’s challenges which improves our mental health. Treating your body with kindness can be especially challenging when it feels like your body has turned against you. Learning to love your body, the actual body you are in with an autoimmune disease can be lifelong work!
Our favorite professionals to learn from in this space are:
- Hilarie McBride – The Wisdom of Your Body
- Dr. Kristin Neff – Self-Compassion Guided Practices and Exercises
9. Resist comparisons
In this social media world, it is so easy to find ourselves scrolling and wanting what someone else seems to have. It might look like other people can eat anything they want and feel great, but that’s rarely true.
Consider unfollowing social media accounts that make you feel bad or deleting social media apps altogether.
10. Learn to listen to how your body wants to move
There are so many ways to exercise, but when we are in the midst of healing, our body craves gentle movement instead of high-intensity training.
- For some folks with an autoimmune disease (especially when you have first been diagnosed and are still struggling with symptoms), this might mean trading in your CrossFit membership for walks or dance parties in your living room.
- It’s important to consider that there might also be days when you shouldn’t exercise at all but rather focus on rest.
11. Rest more
This can be such a hard concept, partially because many of us are taught to think that more is always better and productivity is what matters. We live in this “rise and grind” culture where busyness is seen as the only way to live.
- This is unhealthy, especially so for those with celiac disease. Rest is necessary for healing!
- For you, this might look like laying down for a nap on your lunch break or resting while your little one naps in the afternoon.
- It might even look like restructuring your day (and your priorities) so that you go to sleep earlier.
12. Feel your feelings
This might mean having hard conversations with yourself about what you’re doing to numb your feelings (examples include Netflix binging, drinking too much alcohol, and shopping).
Seeing a counselor or therapist is a great tool to start this process. Common feelings that come up for our clients with autoimmune diseases often include guilt, sadness, and loneliness.
Here are some resources to get you started:
- Permission to Feel is a practical book that helps you understand and even appreciate what you are feeling.
- Psychology Today – the find a therapist tool on this website can help locate a therapist in your area.
13. Practice gratitude
Gratitude practice is a technique that involves focusing on the positive things in your life and expressing appreciation for them. Practicing regularly can help shift your perspective from what you can’t have (like gluten) to all that you do have (family, friends, career success etc). Practicing gratitude reduces feelings of stress and anxiety.
Try writing down three things you are grateful for every night before bed.
14. Address cognitive dissonance
This occurs when you hold two or more contradictory beliefs, attitudes, or values and experience mental discomfort.
Addressing cognitive dissonance can promote self-care because it helps you to align your thoughts and behaviors with your values. When experiencing cognitive dissonance, you might engage in behaviors that contradict their beliefs or values, leading to feelings of guilt, shame, or stress. For example, if you value your health yet continue to eat gluten, you might experience this feeling.
Addressing this involves recognizing the conflict and then taking steps to resolve it by changing your behaviors to align more with your values. This helps reduce stress and gives you a sense of peace.
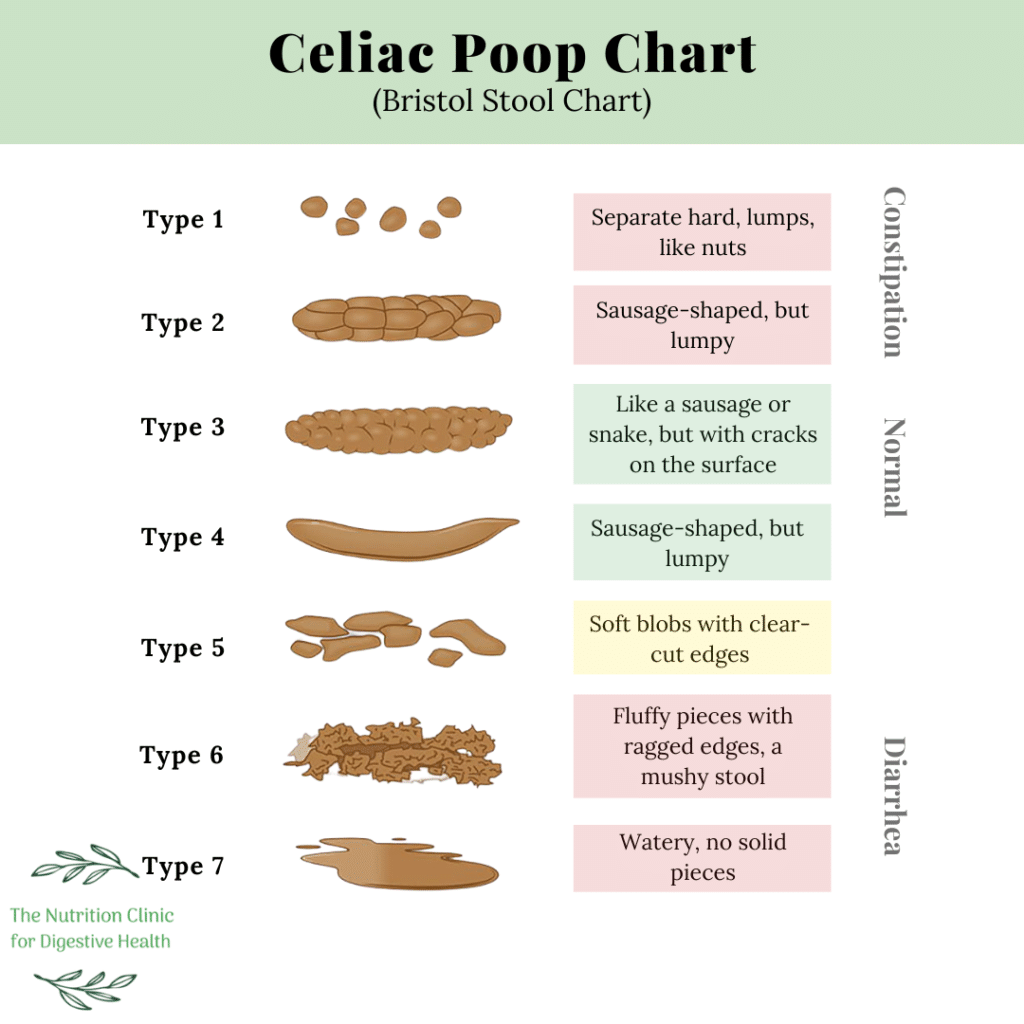
15. Get familiar with the Celiac Poop Chart!
The consistency of your poop is the best indicator of your digestive health! Use the Celiac Poop Chart below to gauge your next bowel movement. Your goal is to have bowel movements at least once, but no more than three times a day, and for them to look like a three or four on the chart below!
Remember your power and agency – It is important to remember that while you can’t change your diagnosis, you still have a lot of agency over your health. You can make informed decisions and proactive choices to care for your body.
How Long After Going Gluten-free Will I Notice a Difference?
When it comes to celiac disease, simply cutting back on gluten won’t be enough to relieve any symptoms. Your symptoms will prevail as long as you’re consuming gluten, even in small amounts. Therefore, cutting gluten out of your diet is the first step in decreasing uncomfortable symptoms of celiac disease.
Most patients with celiac disease will experience some degree of relief from their symptoms within a few days to weeks after completely removing gluten from their diet. When it comes to healing the gut, this can vary from person to person.
Sometimes, it only takes a few weeks to start healing, but oftentimes, it can take the gut three to six months to heal completely if you’re properly repairing the gut at the same time. In some cases, it can take up to two years to fully heal the gut. This is why it is so important to work with a gut health expert when on your celiac disease journey, book a consultation today!
In some cases, doctors may prescribe medications like steroids to help with symptoms of inflammation while your body is healing. This will vary based on symptom severity and individual patient needs.
Conclusion
These self-care tools can help you feel better, but if you’re still feeling poorly after following a gluten-free diet for a while, we recommend working with a dietitian to get individualized support.
Many of our clients with celiac disease need a micronutrient test to address nutrient deficiencies that have occurred because of the damage to the small intestine. People with celiac disease usually have other food intolerances. If removing gluten doesn’t help you feel much better – you might also need to eliminate other foods (we recommend the highly accurate LEAP MRT Test to figure out which ones) that could further exacerbate your chronic inflammation.



Leave a Reply